During the COVID-19 pandemic, telehealth services have proven to be a critical component in connecting patients and care. The Centers for Medicare & Medicaid Services (CMS) expansion of acceptable use of telehealth services has made it easier for providers to get reimbursed for these visits. And more than ever before, doctors and patients alike are open to make use of these services.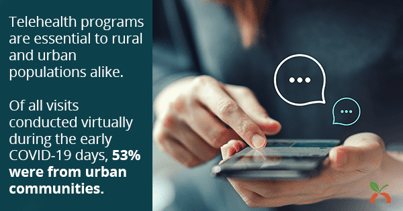
These conditions have created a wave of new telehealth patient visits to manage—and the need for a scalable approach to better understand and serve these remote patient populations. The National Association of Community Health Centers (NACHC) 2020 Factsheet (PDF) details how Health Center Program grantees are providing telehealth services during COVID-19.
Some of the biggest takeaways:

Telehealth program usage is growing rapidly.
During the early months of the pandemic, health and wellness providers embraced telehealth, with the vast majority (98%) of health centers nationwide using telehealth/telephonic services. Prior to COVID-19, only 43% of federally funded health centers used telehealth for a wide range of care delivery or planning. And the health centers that didn’t use telehealth cited specifically the lack of reimbursement, funding, and training as well as inadequate broadband as barriers to usage.
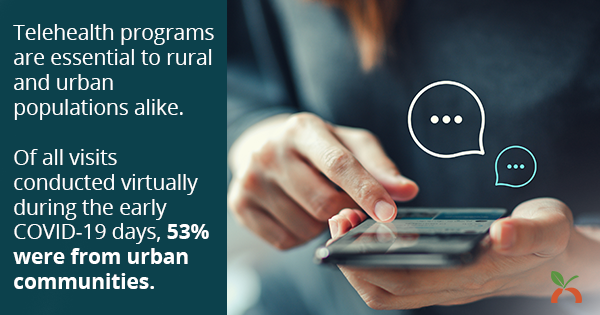
Telehealth programs are essential to rural and urban populations alike.
Of all visits conducted virtually during the early COVID-19 days, 53% were from urban communities.

Telehealth is critical in offsetting the reduction of in-person visits.
The types of care provided allowed patients to continue to receive routine services. Interestingly, when looking at the services that are most commonly provided via telehealth technologies:
- Over 60% of health centers provided mental health services
- Over 30% of health centers provided primary care
- Roughly 20% were services pertaining to chronic conditions
These early findings of telehealth usage during COVID-19 are interesting for a couple reasons. First, the prevalence of mental health telehealth visits shows that the CMS decision to expand the list of covered telehealth services to include therapy services clearly meets a need at this time. Second, these findings indicate that telehealth services are able to fill a gap in providing care for difficult to quantify health conditions—overall wellness, health- and lifestyle-reported health risks, mental health concerns, and the management of chronic conditions. Third, it hints at the future for the delivery of health and wellness services. In a recent survey of specialists by GlobalData, over 74% of physicians said they plan to continue using telehealth when the pandemic wanes.
Gathering HRA Data to Meet the Needs of Your Growing Telehealth Population
COVID-19 has opened the door to telehealth for many healthcare providers. Being able to provide critical preventive care, health management, and mental health services through telehealth has allowed practitioners to reach patients and communities safely and remotely. And an HRA can be a powerful tool in your toolbelt when it comes to better understanding these remote populations.
Coming from the world of health risk assessments (HRAs), I get excited thinking about the types of healthcare services that address these needs. A good HRA is designed to gather the self-reported health data that is often difficult to find in a health chart. Users input their own information, including their health and lifestyle habits, their overall outlook and happiness, and even their readiness to make a change in their health habits.
A telehealth program can use this type of well-being data, combined with biometric health data, to give health and wellness professionals insights into a patient’s risk of developing chronic conditions. This data can also be used to better target patients who will benefit from wellness initiatives, such as improved chronic care management, remote patient monitoring, or behavioral health integration. In fact, Wellsource just teamed up with telehealth provider Certintell for this exact purpose—to close the care gap and support patients in need of chronic care management.
Here’s an example of how HRA data can fuel your telehealth program so you can reach more at-risk individuals: Use your HRA data to identify patients and communities most at risk during COVID-19, and target telehealth programs to help counter those risks. Click here to learn more about using HRA data to identify social determinants of health.
We at Wellsource will continue to follow this topic closely. Because new information and policies are being enacted in this rapidly evolving environment, here are two sources I’ve found helpful in keeping up with the change in telehealth coverage:
- The Center for Medicare & Medicaid Services (CMS) fact sheet of the areas of CMS flexibilities for fighting COVID-19, including in payments for Medicare Telehealth Services (PDF).
- The Center for Connected Health Policy (CCHP) summary of changes the CMS has made to telehealth policy.
And of course, when choosing an HRA solution for telehealth purposes, you may quickly find that not all HRA solutions are equal to the task. A good HRA can easily scale to serve a growing population and provide insights that enable you to predict and prevent costly conditions, all while maintaining a quality patient experience. Wellsource has developed a checklist to help you evaluate if your HRA is positioning you for success.